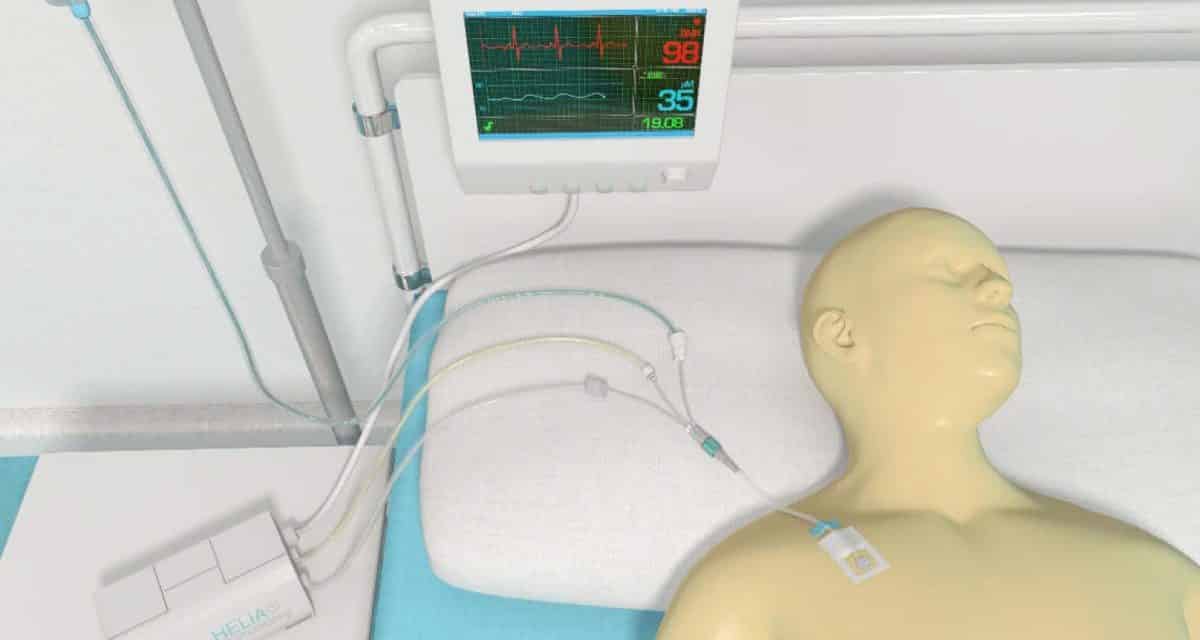
The distinct sound of a heart rate monitor and the trace of an electrocardiogram have become instantly recognizable symbols of medicine. It is almost impossible to imagine a hospital setting without them. Such monitoring of patient’s vital signs – heart rate, blood pressure, temperature – is a key part of clinical practice and enables doctors to track the progress of disease and response to treatment, and to rapidly make life-saving decisions.
The situation is very different with molecular-based measurements on patients. Biomarkers – molecules in the patient’s body associated with disease or with the response to treatment – are typically measured by taking a sample, e.g. a tube of blood, and sending this to a centralized laboratory for analysis. Measuring the concentrations of biomarkers provides insight into the underlying biochemical mechanisms of disease and has become an essential tool in modern medicine. However, these tests generally require logistics and lengthy laboratory procedures, which can be carried out only periodically and introduce delays in the making of clinical decisions.
Helia Biomonitoring, a spin-off company of Eindhoven University of Technology, is developing an innovative technology with the potential to enable the real-time, continuous monitoring of molecular biomarker levels, directly at the patient’s bedside. An example where rapid monitoring of the body’s molecular responses could save lives is in critical care, e.g. for patients who undergo immunological cancer treatment. Such immunotherapies exploit the body’s immune system and stimulate it to attack tumor cells. However, an overactive immune system can in some cases attack healthy cells. This process is characterized by the rapid release of inflammatory biomarkers. Tracking these biomarkers in real time may allow such adverse responses to be detected early and the treatment to be adjusted accordingly.
Helia’s technology, Biosensing based on Particle Motion (BPM), was first described in a Nature Communications paper. The heart of the device is an array of microparticles bound to a surface via nano-scale molecular tethers. The particles move continuously due to thermal fluctuations, constrained by the length of their tethers. The surface and particles are both functionalized with binder molecules specific to the biomarkers of interest, causing transient bonds between surface and particle. Such a binding event pins the particle down and further restricts its movement. This change in the particle motion – caused by the binding of just a single biomarker molecule – can be directly observed.
The binding of biomarker molecules to the surfaces is a reversible, dynamic process. The capture and release events can be monitored over time and used to determine the concentration of the substance of interest. This capability for real-time, reversible observation of binding makes the technology uniquely suited for the continuous monitoring of biomarker levels over hours to days.
The development of a new technology from the research lab toward a clinical device is a difficult and complex journey. In order to accelerate this process, Helia draws on the expertise of the SAFEnmt Open Innovation Test Bed program. The combined knowhow of experts allows challenges to be identified early and addressed efficiently with the support of the consortium.
Key aspects of continuous sensing are the need to establish a robust sensor and a reliable interface to the patient. To enable continuous measurements, membrane-based sampling will be developed so that biomarkers can continuously be measured in a complex biological fluid. The development and testing of the sensor, the fluidic system, and the interfacing will be supported by the Molecular Biosensing group in Eindhoven University of Technology and the Flemish Institute for Technological Research (VITO).
Another key challenge is the availability of reliable and controllable biological model systems for the benchmarking and tuning of the sampling and sensing systems. The model system should mimic the response of the body to disease and intervention, across relevant timescales. Here, continuous cell culture reactors or organ-on-chip will be investigated, supported by the expertise of VITO and of the Biomedical Research Networking Center experts on Bioengineering, Biomaterials and Nanomedicine (CIBER-BBN). CIBER-BBN brings together some of the main Spanish research groups in the field of Bioengineering, Biomaterials and Nanomedicine, including both universities and hospitals and other technological or research centers.
The aim will be to provide test systems which reflect the complex nature of biological samples, but which can be reliably reproduced. Organ-on-a-chip systems are increasingly being investigated as alternatives to animal testing for medical trials. These devices allow tests to be carried out on miniature samples of tissue contained inside a microfluidic chip which still accurately reflect the structure and function of living organs. They can be stimulated to mimic the effects of disease or of treatment, and then their responses can be monitored over time. The miniscule sample volume and high sensitivity of BPM detection will enable the use of these miniature chips as testbeds, facilitating the development and validation of the technology towards its use for future medical applications.
Developing novel medical technologies remains a challenging task, and there is still a lot of work ahead for Helia. We hope that the SAFEnmt test bed will help to accelerate the development of potentially life-saving technologies like Helia’s BPM, for future applications in clinical practice.
Interested in finding out more about Helia’s technology, or about the work of the SAFEnmt partners? Head to the Helia website or leave us a comment below!